You are in the middle of a busy day, and suddenly, an irritating itch starts bothering you down there. It might come with some unusual discharge or a burning feeling that makes simple things like sitting and walking uncomfortable. If you’ve been through this, you might be dealing with a vaginal yeast infection –it’s a most common issue that affects so many female’s. But don’t worry; it’s usually nothing serious and can be fixed pretty easly. In this article, we’ll explore adwanced about vaginal yeast infections in a straightforward way. We’ll talk about what causes them, how to spot the signs, and the best ways to treat and prevent them. By the end, you’ll have the information to understand, this like a pro and feel more in control of your health. Let’s explore in and clear up the confusion around this everyday problem.
What Is a Vaginal Yeast Infection?
A vaginal yeast infection happens when there’s too much of a certain fungus growing in your vagina. their name is Candida, and the most common type is Candida albicans. Normally, your body has a mix of bacteria and yeast living together peacefully in places like your mouth, gut, and vagina. The good bacteria, especially ones called lactobacillus, keep the yeast from getting out of hand. But when something throws off that balance, the yeast can multiply fast, leading to irritation and other troubles.
This isn’t rare at all. In fact, up to three out of four women will get at least one yeast infection in their life, and about half might have two or more. It’s most likely to happen between puberty and menopause because of hormone changes during those years. Kids and older women can get them too, but it’s less common. The good thing is, it’s not a sexually transmitted infection, so you don’t catch it like an STI. Even if you’ve never had sex, you could still get one. However, things like oral sex might sometimes play a role by adding more yeast or causing irritation.
Think of your vagina as a mini ecosystem. When it’s healthy, everything stays in check. But life throws curveballs, and that’s when problems start. Knowing this helps take away the shame – it’s just biology, not something you did wrong.
What Causes These Infections?
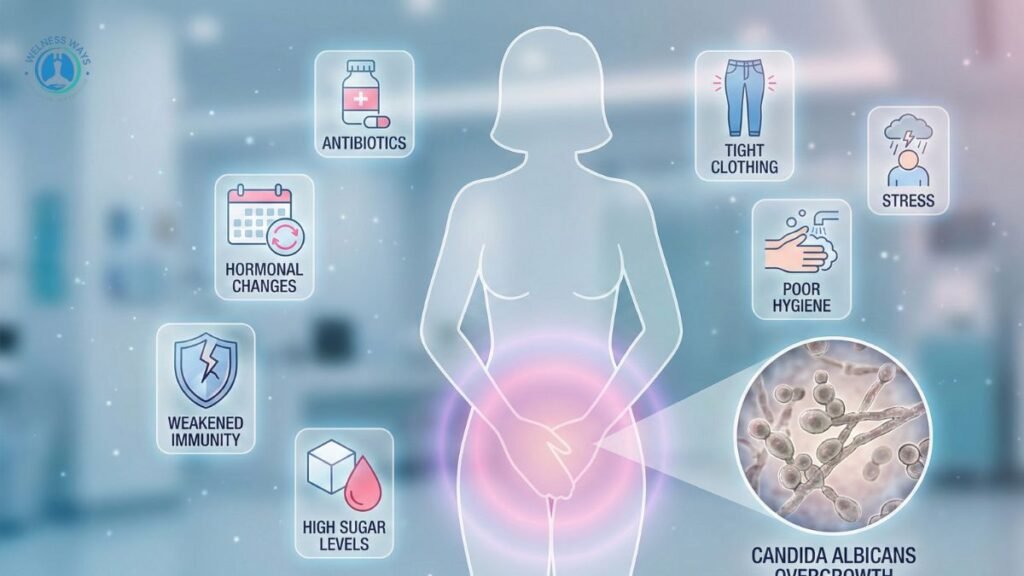
The main reason for a yeast infection is that overgrowth of Candida. But why does it happen? Several things can tip the scales. Antibiotics are a big one. They’re great for killing bad bacteria when you’re sick, but they can also wipe out the good ones in your vagina that control yeast. If you’ve taken antibiotics recently for something like a cold or a UTI, watch out for symptoms afterward.
Hormones matter too. When estrogen levels boost – like during pregnancy, from birth control pills, or even around your period – it can make yeast grow more. That’s why pregnant women often deal with this more. If you have diabetes and your blood sugar isn’t well-controlled, the extra sugar in your body creates a perfect spot for yeast to thrive.
A low immune system is another factor. This could be from illnesses like HIV, or from medicines like steroids that lower your body’s defenses. Everyday habits count as well. Wearing tight clothes that don’t breathe, like synthetic underwear or wet swimsuits for too long, keeps the area moist and warm – yeast loves that. Using scented soaps, douches, or sprays can irritate and disrupt the balance too.
but Sometimes, different types of Candida cause the infection, and those might not respond as well to usual treatments. But most cases are from the common albicans type. Understanding these triggers helps you see it’s often about small changes in your routine or body, not a big mystery.
Also Read- How to Recover Dry Lips in Winter: Best Home Remedies That Actually Work
Spotting the Symptoms
Symptoms can sneak up on you or hit hard. The classic one is intense itching in your vagina and around the vulva – that’s the outer part. It might feel worse at night or after peeing. You could have a burning sensation, especially when you urinate or have sex. The area might look red, swollen, or sore, and on darker skin, the redness might not show as much but the pain is still there.
Discharge is a key sign. It often turns thick, white, and clumpy, like cottage cheese, but without a bad smell. Sometimes it’s watery. Pain during sex or a general soreness can make daily life tough. If it’s really bad – like lots of swelling leading to small tears or cracks in the skin – it might be a more complicated infection. These symptoms can look like other things, like bacterial infections or allergies, so don’t guess – get checked.
Who Is at Higher Risk?
Anyone with a can get a yeast infection, but some people are more prone. If you take antibiotics a lot, your risk goes up because of that bacteria wipeout. High estrogen from pregnancy or hormones boosts chances too. Poorly managed diabetes means more sugar for yeast to feed on.
If your immune system is weak – maybe from meds or health conditions – you’re more vulnerable. Habits like douching wash away good bacteria, and tight, non-breathable clothes create a yeast-friendly environment. Knowing your risks lets you make smart changes to stay ahead.
Also Read- Home Remedy for Cold and Sore Throat: Natural Ways That Actually Work
How Do Doctors Diagnose It?
If you think you have one, see a doctor, especially if it’s new. They’ll ask about your symptoms and history, then do a quick pelvic exam to check for redness or discharge. They might take a sample of discharge and look at it under a microscope to see yeast cells or hyphae – those are like fungus threads. Sometimes, they send it to a lab for a culture to confirm the type. This rules out other issues like bacterial vaginosis or STIs. It’s fast and helps get the right treatment.
Treatment Options That Work
Good news: Most yeast infections clear up with antifungal meds. For simple ones, over-the-counter creams or suppositories like miconazole (Monistat) or clotrimazole work in 1 to 7 days. You apply them inside the vagina or on the vulva. A single oral pill like fluconazole (Diflucan) is another option – just one dose often does it.
For tougher cases – like if you get them often (four or more a year), they’re severe, or you have diabetes – you might need longer treatment, like 7 to 14 days of cream or multiple pills. Recurrent ones could mean weekly meds for months to keep them away. During treatment, skip sex to avoid more irritation, and know some creams can weaken condoms. Symptoms usually ease in a few days, but finish the whole course.
If it’s not albicans yeast, like Candida glabrata, standard stuff might not work, so doctors might try boric acid capsules or other options. Always talk to a pro for the best plan.
Home Remedies: Helpful or Hype?

Some people try natural fixes, but they’re not as strong as meds. Eating yogurt with live cultures or taking probiotic supplements might help restore good bacteria, but evidence is mixed. Coconut oil has antifungal properties in tests, but applying it vaginally isn’t proven safe or effective for everyone – it could irritate.
Tea tree oil is another one, but dilute it a lot and test first, as it can burn. Garlic? Skip inserting it – no good proof, and it might hurt. A gentle saltwater rinse could soothe itching short-term, but it won’t cure anything. Home stuff is okay for mild relief, but see a doctor for real treatment, especially if symptoms stick around.
Preventing Yeast Infections in Daily Life
Prevention is easier than you think. Choose cotton underwear that lets air flow and change out of wet clothes fast after swimming or working out. Skip douching – it removes helpful bacteria. Avoid scented products like soaps or pads that irritate.
If you have diabetes, keep blood sugar steady. Use antibiotics only when needed, and maybe add probiotics during them. Wipe front to back after the bathroom to avoid spreading germs. Loose clothes help too. These small steps can cut your risk a lot.
Possible Complications to Watch For
Usually, yeast infections are no big deal, but if ignored, they can cause bad irritation, skin breaks, or even spread a bit. In people with weak immune systems, they might get worse or happen more. Recurrent ones can mess with your life, causing ongoing discomfort or stress. During pregnancy, untreated ones might raise risks like early birth, so get treated fast. But with quick care, complications are rare.
When Should You See a Doctor?
Don’t wait if it’s your first time, symptoms are severe, or they don’t go away with OTC stuff. If you’re pregnant, have diabetes, or a weak immune system, check in right away. Fever, bad pain, or weird smells might mean something else. Recurrent infections need a doc to find underlying issues.
Common Myths Busted
Myth: Yeast infections mean you’re not clean. Fact: They’re from imbalances, not dirt.
Myth: They’re always from sex. Fact: Sex can help spread, but many happen without it.
Myth: Strong odor is normal. Fact: No, that’s more like bacterial infections.
Myth: Men can’t get them. Fact: They can, but it’s rarer and shows as balanitis.
Clearing these up reduces worry.
Special Cases: Pregnancy, Diabetes, and More
In pregnancy, higher hormones make infections common, but only use topical treatments – no oral pills to avoid baby risks. For diabetes, good sugar control is key. If you have HIV or are on immune-suppressing meds, infections might be harder to beat and need longer care. Tailor your approach based on your health.
Comparing Vaginal Infections: A Quick Table
To help tell yeast infections apart from similar issues, here’s a simple table:
| Infection Type | Main Symptoms | Discharge | Odor | Common Causes |
|---|---|---|---|---|
| Yeast Infection | Itching, burning, soreness | Thick, white, clumpy | Little/none | Antibiotics, hormones |
| Bacterial Vaginosis | Thin discharge, itching | Grayish, thin | Fishy | Bacterial imbalance |
| UTI | Burning urination, frequent pee | None or cloudy urine | None | Bacteria in urinary tract |
| Trichomoniasis | Itching, soreness, frothy discharge | Greenish-yellow, frothy | Bad | Parasite from sex |
This table shows key differences – always get tested for sure.
Wrapping Up: Empowering Your Health Choices
Vaginal yeast infections are a hassle, but armed with this info, you can spot them early, treat them right, and prevent most. Remember, your body is amazing at balancing itself, but sometimes it needs a little help. Listen to it, make those easy lifestyle tweaks, and don’t hesitate to seek professional advice. Staying informed means less stress and better days ahead. You’ve got this!
Disclaimer: This article is for general information only and is not meant to replace medical advice. Symptoms can vary, and self-diagnosis isn’t reliable. Always talk to a healthcare provider for proper diagnosis, treatment, or if you have concerns. The info here comes from reliable sources but isn’t personalized. If you’re pregnant, have ongoing health issues, or symptoms worsen, get professional help right away.

